What is a Total Knee Replacement?
A Total Knee Replacement (also called Total Knee Arthoplasty) is a surgical procedure designed to replace the severely diseased knee joint with an artificial knee joint.
It involves removing parts of your femur (thigh bone), tibia (shin bone) and patella ( kneecap) and replacing them with a combination of surgical-grade metal alloys and highly wear resistant plastic.
It’s designed to help with pain and restore the bending movement of the knee.
-
What is Computer Navigation?
During a joint replacement procedure, it is important that everything is aligned properly. Accurate alignment of the knee components is critical to the overall function of your new joint and it also plays a role in helping your joint feel healthy again, and helping the joint replacement to potentially last longer.
A common alternative to computer navigation are patient specific implants where the alignment is assessed and calculated by computer tomography (CT) prior to surgery rather than intraoperative computer navigation or alignment jigs. The decision is based on patient anatomy and complexity of the surgery required.
Computer-assisted technology has made it possible for your orthopaedic specialist to navigate joint replacement procedures with a level of accuracy so precise it may improve the results of your surgery.

Potential Benefits of Computer-Assisted Surgery
There are several potential benefits for those who have computer-assisted surgery with their total joint replacement:
Designed to place joint replacement implants with precision, which
- May increase the life of your replacement
- Reduces the risk of dislocation and revision surgery
- Results in greater stability and range of motion
- Helps improve the overall function of your joint replacement
How does it work?
Computer Navigation technology uses special tracking devices, providing a comprehensive understanding of your joint mechanics in the operating room (OR). Armed with this information, adjustments within a fraction of a degree, helping to ensure your new joint has the stability and range of motion needed for a successful replacement. Specifically, the technology uses the latest advancements in science and computer engineering to make the procedure more accurate than joint surgery without it.
As an instrument is moved within your joint, special infrared trackers calculate its position and wireless instruments instantaneously transfer the data to a computer in the OR. This information is then displayed on a monitor as an interactive model of the anatomy or “blueprint” that supplies all the angles, lines and measurements of your unique anatomy. Your diseased bone is then replaced with new, artificial joint components often called prostheses or implants. Joint implants are engineered to replicate a normal, healthy joint.
Why is an accurately implanted knee replacement necessary?
Implant misalignment, even if only by a few degrees, requires some patients to have additional surgery within a few years, either to reduce discomfort or to replace the worn implant. For most patients, the most dramatic benefit of a well aligned implant is the return to normal mobility and an improved quality of life.
-
Who is knee replacement surgery for?
The most common reason for a Total Knee Replacement is severe pain and dysfunction caused by knee arthritis.
There are many types of arthritis but by far the most common type of arthritis that benefits from a Total Knee Replacement is Osteoarthritis, followed by Rheumatoid Arthritis.
Osteoarthritis is a wear and tear process that happens with aging but can also occur after an injury to the knee joint.
 Diagram of a knee with Osteoarthritis
Diagram of a knee with OsteoarthritisIf you are considering total knee replacement surgery, you should have first tried non-surgical methods to help you with your knee pain. These include:
- pain medications
- using a walking stick or other walking aid
- exercises to maintain the movement and stength of the knee and the muscles around the knee
- maintaining a healthy weight or loosing weight if necessary
- some people gain benefit from using a knee brace
Your surgeon may suggest that you have a knee replacement if you have:
- Severe pain. A knee replacement is a big operation and should only be considered if the pain in your knee is severe. For example, your pain should make it difficult to walk, climb stairs and perform your activities at home.
- Severe dysfunction. Your knee pain should be affecting your mobility and often causes stiffness and prevent you from fully bending or straightening your knee.
- Tried other ways of controlling your pain. You’ve tried other methods to improve symptoms, for example, resting, weight loss, physiotherapy, a cane or other walking aid, medications and knee braces, but they’ve failed.
- Be Old enough. It is best to perform a knee replacement when your older, for example over 60. This is because knee replacements can wear out and eventually fail. Total knee replacements often last over 15 – 20 years, so ideally, you have a total knee replacement that will last the rest of your life. If you are younger, Dr Tran may suggest other operations such as:
- knee arthroscopy,
- knee straigthening / realigning procedures called osteotomies
- partial knee replacements
- Also, young physically active people are much more likely to prematurely wear out the Total knee replacement.
- Be Fit Enough for the Operation. A knee replacement is major surgery and can put alot of strain on your body. If you have conditions such as blocked arteries, diabetes, or are extremely obese, you have a increased risk of complications. There are some people who are not fit enough to have a knee replacement.
What are the benefits of the operation?
A knee replacement can dramatically reduce the pain caused by arthritis and get you walking and bending your knee again.
A knee replacement may not remove all your pain or fully restore your knee movement, and it will not make your knee ‘brand new’ again. But it will considerably reduce your pain.
 A Xray of the Right Knee showing Osteoarthritis
A Xray of the Right Knee showing Osteoarthritis A Xray of the Right Knee showing normal anatomy
A Xray of the Right Knee showing normal anatomyRisks of not having the surgery
Knee replacement is elective surgery, so should be considered carefully after considering the operation, it’s pros and cons and the alternatives. However, knee arthritis is a progressive disorder and the pain can be become so severe that it stops you performing everyday activities such as walking, climbing stairs, showering, gardening and shopping. You may no longer be independent and able to look after yourself.
-
Complications
The risks and complications of a knee replacement include:
- Infection. This may require antibiotics, further surgery and possibly the new knee joint to be removed, and possible the leg amputation. Wound infection in about 1 in 100 people Infection is a major complication and may require further surgery and possibly the new knee joint to be removed and possibly the leg amputated. Infection to the prosthesis via the bloodstream in the following years after replacement surgery. The knee joint may have to be removed.
- Deep Vein Thrombosis and Pulmonary Embolism. Blood clots can form in the legs. The clots can break off and travel to the lungs and can cause death. Blood clots can form in the legs. If untreated, this can happen in 1 in 5 people. The clots can break off and travel to the lungs in 1 in 100 people, and can cause death in 1 in 3,000 people.
- Wear and Tear. The artificial joint may fail or wear out. Surgical revision of the knee joint replacement may be required. The artificial joint will loosen or wear out This can happen over a period but 9 out of ten knee joint replacements are still working after 10 years. Surgical revision of the knee joint replacement may be required.
- Dislocation of the knee joint The knee joint/patella can dislocate because muscles and ligaments have not yet repaired themselves to provide support to the joint. Re-operation is required.
- Numbness. Numbness at the side of the cut can happen. This may be temporary or permanent. Numbness at the side of the cut can happen This may be temporary or permanent.
- Nerve damage. Damage to the peroneal nerve around the knee during surgery. This may be temporary or permanent. Further surgery may be necessary. Damage to the nerves may cause a burning pain and inability to straighten the leg. A nerve block may be used to relieve the pain and the leg manipulated. Numbness/ paralysis of the foot. Damage to the peroneal nerve around the knee during surgery in 1 in 300 people. This may be temporary or permanent. Further surgery may be necessary.
- Stiffness. Stiffening of the knee after the surgery causing difficulty in walking and sitting and pain on movement. Manipulation and possibly further surgery may be required. Stiffening of the knee causing difficulty in walking and sitting and pain on movement in 1 in 60 peoplex. Manipulation and possibly further surgery.
- Fracture. The bones around the joint may break during or after surgery. A plaster may be required to repair the break or further surgery may be required. The bones around the joint may break during or after surgery. This can occur in 1 in 40 to 1 in 300 cases depending on bone strength. A plaster may be required to repair the break or further surgery may be required.
- Patella Fracture. The kneecap may break The kneecap may break in 1 in 650 people.v Further surgery may be required to repair the knee cap.
- Damage to blood vessels. Damage to the blood vessel behind the knee during surgery. Surgery on the blood vessel will be needed and sometimes leg amputation. Loss of blood supply to the leg Damage to the blood vessel behind the knee in 1 in 300 to 1 in 500 people. Surgery on the blood vessel, and sometimes leg amputation.
- Scar. In some people, healing of the wound may be abnormal and the wound can be thickened and red and the scar may be painful.
- Death. Death is extremely rare due to knee replacement.
- Infection around the prosthesis years later Infection can spread to the replaced joint via the bloodstream for years after replacement surgery (1 in 300 people). The knee joint may have to be removed. To prevent this, you will need antibiotics before other procedures and dental work.
- Smokers. Increased risk in smokers. Smoking slows wound healing and affects the heart, lungs and circulation. Giving up smoking before operation will help reduce the risk. An increased risk of wound infection, chest infection, heart and lung complications, blood clots and pulmonary embolism.
-
Before the Operation
Preparing for Surgery
Before your operation, your fitness for the operation will be assessed and all the necessary tests performed in preparation for the operation.
During the visit, you will be seen by a
- physician
- nurse
- anaesthetist (if necessary)
Tests
Tests that may be ordered for you include:
- blood tests: FBE, U&E
- Xray of your knee
- Urine Test
- ECG
- CT Scan of your knee if you are having a Patient Specific Instrumentation (PSI) knee replacement
Preparing Your Skin
Your skin should not have any infections or irritations before surgery. If either is present, contact your surgeon for a program to improve your skin before surgery.
Medications
Your surgeon or physician will advise you which medications you should stop or can continue taking before surgery.
Go see your dentist
Consider getting treatment for significant dental diseases (including tooth extractions and periodontal work) before your knee replacement surgery. Routine cleaning of your teeth should be delayed for several weeks after surgery.
Get some help from your friends and family
Although you will be able to walk with crutches or a walker soon after surgery, you will need some help for several weeks with such tasks as cooking, shopping, bathing, and laundry. If you live alone SOS clinic, a social worker, or a discharge planner at the hospital can help you make advance arrangements to have someone assist you at your home. A short stay in an extended-care facility during your recovery after surgery also may be arranged.
Home Planning
The following is a list of home modifications that will make your return home easier during your recovery:
- Securely fastened safety bars or handrails in your shower or bath
- Secure handrails along all stairways
- A stable chair for your early recovery with a firm seat cushion (that allows your knees to remain lower than your hips), a firm back, and two arms
- A raised toilet seat
- A stable shower bench or chair for bathing
- A long-handled sponge and shower hose
- A dressing stick, a sock aid, and a long-handled shoe horn for putting on and taking off shoes and socks without excessively bending your new knee
- A reacher that will allow you to grab objects without excessive bending of your knees
- Removal of all loose carpets and electrical cords from the areas where you walk in your home
-
During the Operation
An incision that is typically around 15 – 25 cm. It usually runs straight down the middle of the front of your knee.
Precise surgical bone cuts are made at the end of your femur (thigh bone) and the top of your tibia (shin bone), thereby removing your arthritic knee joint.
The knee replacement is made of surgical grade metal alloy and plastic.
It is inserted and held inplace either by surgical cement, a special coating on the metal or screws.
The operation takes 2 – 4 hours.
At the time of surgery and for a short period after your surgery, you will be given antibiotics and medications to thin your blood.


-
After the Operation
After the operation, the nursing staff will closely watch you until you have recovered from the anaesthetic. You will then go back to the ward where you will recover until you are well enough to go home, usually 7-10 days after surgery.

A Xray of a knee with a Total Knee Replacement
-
Recovery and Rehabilitation
Once your arrive on the ward, a team of nurses, physiotherapists, occupational therapists and doctors, will help you recover from your operation.
My Pain
You can expect to have pain in the operation site. You will have either:
- An injection into your spine – an epidural – which may be connected to a fine tube and a pump which sends painkiller into your spine. This can cause headache and soreness at the injection.
- A patient controlled analgesia which, when you press a button, releases a painkiller into your IV drip. This can cause nausea and vomiting, sleepiness, and/ or trouble emptying your bladder. These pain-killing devices will stay in for 24 – 48 hours depending on the amount of pain you have.
My Food
You may have a drip in your arm, this will be removed by the second day after your operation. To begin with, you can have small sips of water, then slowly take more until you are eating normally.
My Wound
Your wound will be a cut about 20 to 30 cms down the front of your leg from above to below the knee and will be closed with either stitches or clips. The stitches or clips will stay in for 10 to 14 days. A dressing will cover the cut and you will have a drain to drain any blood and fluid from the wound into a small bag. This is removed 24 to 48 hours after operation – or once the drainage has stopped. You can shower 1 or 2 days after surgery. A waterproof dressing will be put on over the top. Your dressings will be changed as ordered by the surgeon. You may go home with a dressing covering your wound until your stitches or clips are removed. Continue to keep your wound clean and protected until healed and no seepage is present.
My lungs and blood supply
It is very important after surgery that you move as soon as possible. Pump your feet backwards and forwards and bend and straighten your non- operated leg at the knee. This prevents blood clots forming in your legs and possibly travelling to your lungs. This can be fatal. You will be shown which of your pre–operation exercises to continue after surgery. You will start walking the second day after surgery with the use of walking aids. You will be told when you can put your full weight on your new knee. Also, you need to take ten deep breaths every hour, to prevent secretions in the lungs becoming stagnant. If this happens, you may develop a chest infection. At all costs, avoid smoking after surgery as this increases your risk of chest infection.
My Exercises
You will feel tired for a few weeks after surgery. You need to take things easy and return to normal duties, as you feel able to. It takes about 3 months to recover. You will be given exercises to do for a month after your surgery. You will also be shown how to safely climb stairs, shower, dress and toilet yourself.
There are a number of movements to avoid:
- Avoid jumping – even from low surfaces.
- Avoid sudden jolts to the leg (e.g. stepping off kerbs).
- Avoid gaining weight, which puts extra stress on your joint.
- Keep to low – key activities at work and at recreation.
- Avoid kneeling on your new knee joint.
- Be careful in slippery, cluttered or uneven areas so that you don’t fall.xiii You will be told about these before you go home.
Looking after my knee joint
Joint replacements can become infected at any time after the surgery from the first postoperative day to many years down the line.
You can take the following steps to help prevent infection:
- Take antibiotics before dental or any medical procedure.
- See Dr Phong Tran to treat all suspected urinary tract infections.
- Look for signs of infection in the knee including pain, redness, swelling or increased warmth.
- Your new joint replacement may trigger airport metal detector alarms. We will give you a certificate that verifies that you had a knee replacement.
- Keep in mind that you need to protect your knee replacement to ensure a long lasting, successful result. Follow all instructions concerning any activity restrictions.
-
FAQ’s
What are the alternative treatments to having a knee replacement?
Walking aids such as a walking stick. An exercise program can strengthen the muscles around the knee joint and sometimes improve positioning of the knee and relieve pain. Nonsteroidal anti-inflammatory drugs, or NSAIDs. Some common NSAIDs are aspirin, ibuprofen and cerebrex. Corticosteroids such as prednisone or cortisone reduce joint inflammation but can cause further weaken the bones in the joint. Side effects from corticosteroids are increased appetite, weight gain, and lower resistance to infections. Osteotomy. The surgeon cuts the bone away at a point from the damaged joint and restores the joint to its proper position, which helps to load weight evenly across the joint. For some people, an osteotomy relieves pain. Recovery from an osteotomy takes 6 to 12 months. The function of the knee joint may get worse and the patient may need more treatment.
Are there important things I need to tell my doctors?
- Redness, swelling or warmth around the cut
- Leakage from the cut
- Fever and chills.
- Severe knee pain that is not relieved by prescribed painkillers.
- Sudden sharp pain and clicking or popping sound in the knee joint
- Loss of control over leg movement
- Loss of leg movement
- Further surgery planned for the future i.e. dental work, bladder catheterisation, examinations of the bowel, bladder, rectum or stomach.
What are the bones of the knee?
The knee is a hinge joint, formed by the end of the thighbone (femur) and the end of the shin bone (tibia). The bones are coated in cartilage, which acts as a cushion between the two bones and allows the knee to move. In front of these bones is the kneecap (patella) which glides in a groove on the end of the thigh bone.

Diagram of the bones and ligaments of the knee
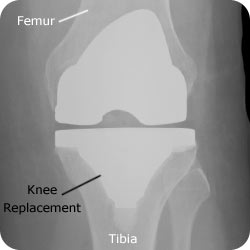
Xray of a knee with a total knee replacement (cemented variety)
Computer Navigation
Improving the accuracy of your knee replacement.
Knee Navigation uses an infrared device and instruments to assist the surgeon in aligning the knee implant.
The surgeon’s cuts into the bone can be guided to within one degree of surgical accuracy.
which means Better patient outcomes
Knee replacement surgery
also known as
– total knee replacement
– TKR
– knee arthroplasty
